The devastating impact of Alzheimer’s disease has long perplexed scientists and medical professionals, with no effective treatment yet available. However, a groundbreaking study has recently confirmed the role of the gut microbiome in the development of this debilitating condition. Researchers from around the world have successfully demonstrated that memory impairments associated with Alzheimer’s can be passed on to healthy rats through gut microbiota transplants. Moreover, specific bacteria in the gut have been directly linked to cognitive decline in Alzheimer’s patients. These findings uncover the gut microbiome as a critical area for further research in Alzheimer’s and other forms of dementia, potentially paving the way for novel treatment approaches.
Traditionally, individuals with Alzheimer’s have been diagnosed at or after the onset of cognitive symptoms. However, such timing may prove to be too late for the current therapeutic methods. Neuroscientist Yvonne Nolan from the University College Cork suggests that exploring the role of gut microbes during the early stages of dementia, known as prodromal, could open up new possibilities for therapy development or even individualized interventions. Understanding how gut microbiota contribute to the progression of Alzheimer’s before symptoms appear could revolutionize the way we approach this devastating disease.
Gut Microbiota as a Potentially Causal Factor
Previous evidence has hinted at changes in the gut microbiota as a potential risk factor for Alzheimer’s development, although it remained unclear whether the association was merely coincidental. The recent study, however, provides confirmation that the gut microbiota play a causal role in triggering symptoms of this neurodegenerative disease. Sandrine Thuret, a neuroscientist at King’s College London, acknowledges the significance of this research, stating that it represents an important step forward in our understanding of Alzheimer’s.
Researchers from the University College Cork, King’s College London, and IRCCS Saint John of God Clinical Research Centre of Brescia conducted a comprehensive study to unravel the influence of gut microbiota on brain health and behavior in Alzheimer’s patients. The study involved human participants, including both Alzheimer’s patients and healthy controls, who provided blood samples for research purposes. Additionally, stool samples were collected from some participants to obtain their gut microbiota. The researchers then transplanted gut microbiota from Alzheimer’s patients into young adult rats whose microbiomes had been depleted by antibiotics. A matching group of rats received gut microbiota from individuals in the healthy control group.
Impaired Memory Behaviors and Hippocampal Neurogenesis
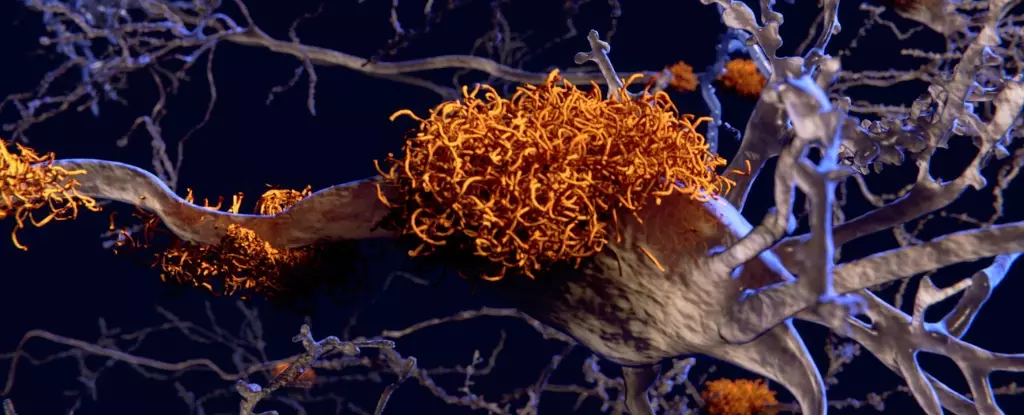
Behavioral tests were conducted on the transplanted rats to evaluate memory performance and other traits associated with Alzheimer’s disease. The results were striking. Rats that received gut microbiome transplants from Alzheimer’s patients displayed impaired memory behaviors, particularly those related to adult hippocampal neurogenesis. Neurogenesis is the process of generating new neurons in the hippocampus, a region crucial for memory and mood regulation, and one of the earliest areas affected by Alzheimer’s.
According to Yvonne Nolan, the lead researcher, “The memory tests we investigated rely on the growth of new nerve cells in the hippocampus region of the brain. Animals with gut bacteria from people with Alzheimer’s produced fewer new nerve cells and had impaired memory.” Interestingly, the severity of impairments in hippocampal neurogenesis was more pronounced in rats receiving gut microbiota from Alzheimer’s patients with lower cognitive test scores.
The researchers also observed notable changes in the rats’ hippocampal metabolome, which consists of metabolites involved in cell maintenance, growth, and normal function. These modifications in the metabolome could contribute to the decreased growth of new neurons in the hippocampus. Although measuring hippocampal neurogenesis is challenging in living humans, neurogenesis in human neural stem cells decreased when exposed to blood from Alzheimer’s patients. Furthermore, the levels of gene expression in stem cells exposed to the blood of Alzheimer’s patients correlated with their cognitive test performance and the types of bacteria present in their gut.
Future Directions and Considerations
The study revealed that Alzheimer’s patients had significantly lower levels of bacteria from the genus Coprococcus, known for promoting healthy aging. Additionally, they exhibited an increase in bacteria from the Desulfovibrio genus, consistent with previous studies on animal models of Alzheimer’s and Parkinson’s disease.
To expand our understanding further, future investigations should thoroughly assess other factors influencing gut microbiota, such as health status, lifestyle, and medication history. Such a comprehensive approach will allow us to decipher the intricate relationship between the gut microbiome and Alzheimer’s disease fully.
The confirmation of a causal link between gut microbiota and Alzheimer’s disease is an extraordinary breakthrough in the field of neurodegenerative research. By demonstrating that memory impairments associated with Alzheimer’s can be passed on through gut microbiota transplants, this study highlights the vital role of the gut microbiome in the development of the disease. These findings open up new possibilities for therapeutic interventions and bring hope to millions of people affected by Alzheimer’s and other forms of dementia. As we delve deeper into the intricate connection between the gut and the brain, we may unlock the key to preventing and treating Alzheimer’s disease.


Leave a Reply