In a groundbreaking discovery, scientists at Weill Cornell Medicine in the United States have repurposed human stomach cells into tissues that release insulin in response to rising blood sugar levels. This discovery has the potential to provide an effective way to manage conditions such as type 1 diabetes. The experiment involved transplanting gastric insulin-secreting (GINS) cells into mice, which reversed diabetes. The pancreas is responsible for releasing the hormone insulin in response to high sugar levels in the blood. In people with diabetes, these tissues are damaged or die off, compromising their ability to move glucose into cells for fuel. Although GINS cells are not beta cells, they can mimic their function. The gut has many stem cells that can transform into different cell types and proliferate quickly. The hope is that people with diabetes can have their own gut stem cells transformed into GINS cells, which would limit the risk of rejection.
Efficient Reprogramming Process
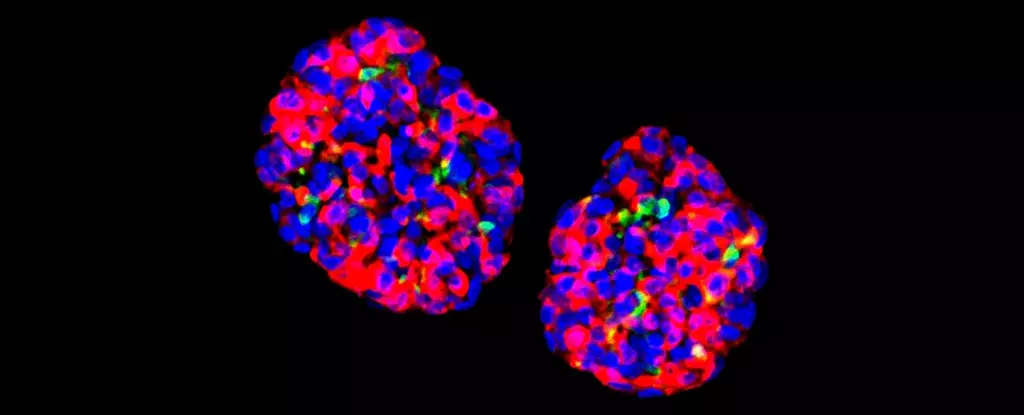
Scientists have been trying to achieve this breakthrough for many years, but without any real success. In the current investigation, the team activated three specific proteins in the cells that control gene expression in a particular order to trigger the transformation into GINS cells. The reprogramming process is highly efficient, and when the cells were grown in small clusters known as organoids, they showed sensitivity to glucose. They were then able to show long-lasting effects on diabetes in mice. The researchers noted that producing GINS cells from stomach cells is not a complicated process and only takes a few days. Furthermore, these new organoids can last for many months after being transplanted.
Promising Initial Results
The insulin hormone is crucial in regulating blood glucose, and without sufficient levels, people run the risk of a variety of health complications. Millions of people worldwide live with diabetes, mostly using insulin injections to help keep glucose levels under control. Although it is still early days for this approach, it would enable the body to manage insulin levels more naturally again. The researchers noted several differences between human and mouse stomach tissue that need to be addressed in future studies. The GINS cells also need to be made less vulnerable to immune system attack. Nevertheless, initial signs are promising. The research adds to a number of ways scientists are looking to tackle diabetes, including diet improvements and tweaking the way that insulin is delivered to the body. Joe Zhou, an associate professor of regenerative medicine at Weill Cornell Medicine in New York, said, “This is a proof-of-concept study that gives us a solid foundation for developing a treatment, based on patients’ cells, for type 1 diabetes and severe type 2 diabetes.”


Leave a Reply