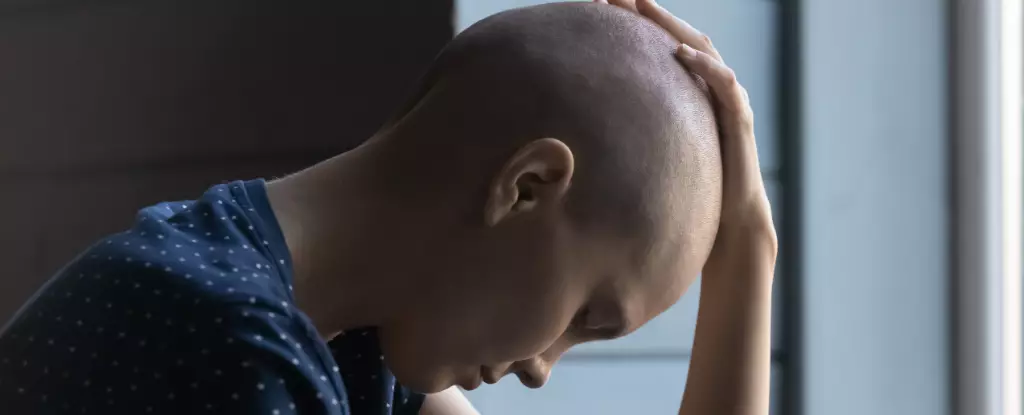
Cancer, often perceived solely as a physical affliction, embeds deeper psychological shadows within its victims, particularly in the advanced stages of the disease. One of the most heartbreaking aspects of this struggle is the phenomenon of apathy, a profound sense of disengagement from life that affects nearly 80% of patients experiencing late-stage cancers. As they navigate through their treatments and face the daunting realities of their illness, these patients often lose interest in activities that once brought them joy, retreating into a shell of isolation that not only hampers their recovery but also alienates them from loved ones. Apathy in cancer isn’t simply an emotional byproduct of suffering—it’s a biological response that stems from the very dynamics of the disease.
Understanding Cachexia’s Grip
Central to understanding this apathy is the syndrome known as cachexia, which is not just about weight loss but an all-encompassing metabolic derangement that strips away not just physical strength but also the psychological stamina necessary for engaging in life. Patients, despite receiving adequate nutrition, experience debilitating muscle wasting and energy depletion. They appear fragile, and more importantly, they seem to lose the spark of drive and ambition that motivates human interaction and personal engagement. The prevailing assumption among clinicians has often been that this loss is merely the result of an understandable psychological reaction to the ravaging effects of cancer. However, new research suggests that apathy may actually be a core symptom—an active part of how cancer operates.
The Brain’s Inflammatory Response
Recent studies conducted on mouse models have provided astonishing insights into the relationship between cancer and the brain’s motivation pathways. These investigations have revealed a critical brain region known as the area postrema, which acts as an inflammation sensor. As tumors grow, they release cytokines into the circulatory system. The area postrema, bypassing the protective blood-brain barrier, directly detects these harmful signals. In response, it initiates a cascading failure that results in a marked decline in dopamine—the neurotransmitter that fuels motivation and desire to act. This process unveils a chilling reality: cancer not only attacks the body; it subtly manipulates the brain’s wiring to diminish an individual’s will to fight back or even engage in basic human activities.
Behavioral Evidence of Motivation Decline
Interestingly, experiments designed based on behavioral economics shed light on how this neurological decline manifests behaviorally. In experimental setups where mice were tasked with reaching rewards, a disturbing trend emerged as cancer progressed: the mice, although still willing to pursue simple rewards, increasingly abandoned tasks that required more effort. Observing real-time dopamine levels allowed researchers to connect the dots between biological declines and behavioral outputs, aligning perfectly with what cancer patients often voice: “Everything seems insurmountably difficult.” The implications of such findings are profoundly concerning; as the disease advances, both the physical and mental realms devolve in a synchronized symphony of suffering.
Reviving the Spark of Motivation
On a more hopeful note, the same studies exploring the brain’s responses have identified potential therapeutic pathways that may restore motivation even amid the progression of the disease. By either genetically manipulating the neurons in the area postrema or inhibiting specific inflammatory pathways using existing drug formulations, researchers have demonstrated remarkable success in reviving motivation in experimental mice afflicted with cancer cachexia. Such interventions, though still in their infancy when it comes to human application, highlight a beacon of hope for cancer patients and their families, suggesting that innovative treatments could change the trajectory of how we approach the supportive care of patients.
Broader Implications Beyond Cancer
The significance of these findings resonates far beyond cancer alone. The inflammatory pathways that suppress motivation are not unique to oncological conditions; similar mechanisms may underpin apathy in various chronic illnesses, including autoimmune disorders and even mental health conditions like depression. Apathy, initially viewed as a natural protective evolution response to acute illness, may become counterproductive when subjected to the relentless grip of chronic inflammation. The lessons learned from cancer research could illuminate paths to understanding and treating motivational deficits in a multitude of chronic ailments.
In wrapping our minds around the findings of this intriguing research, we must acknowledge the intricate ties between physical ailment and psychological health. By targeting the inflammatory signals hijacking our motivational centers, we may reclaim not just the physical but the very essence of personhood itself, rekindling hope where it may have been extinguished. As families witness their loved ones slip into apathy, understanding these biological underpinnings presents a powerful allure—a reminder that humanity and determination are not merely a matter of will but are intricately woven into the fabric of our biology. The promise of innovations in treating these disheartening symptoms galvanizes a pursuit of healing that transcends the disease itself.

Leave a Reply