Anorexia nervosa, a complex and multifaceted mental health disorder, continues to baffle researchers and healthcare professionals alike. Characterized by an incessant fear of gaining weight, distorted body image, and severely restricted eating behaviors, individuals suffering from this condition face dire consequences, including severe anxiety, depression, and malnutrition. Recent studies shed light on the neurobiological mechanisms that may underpin anorexia, suggesting that neurotransmitter dysfunction plays a pivotal role in its development and manifestation.
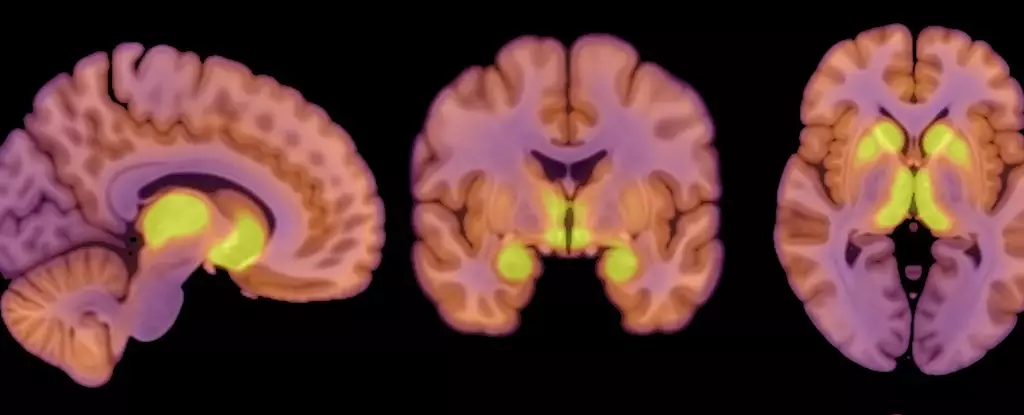
The mechanics of anorexia nervosa have long been the subject of intense investigation, yet many aspects remain elusive. A recent study has brought forward the potential involvement of neurotransmitter systems in the condition’s pathology. The focus has been drawn particularly to the mu-opioid receptors (MORs) in the brain. This class of receptors is intricately linked to the opioid system, which plays a fundamental role in regulating both appetite and pleasure. According to the findings of this research, there is a substantial increase in MOR availability in individuals with anorexia nervosa, particularly in brain regions associated with reward processing.
Researchers, led by physiologist Pirjo Nuutila at the University of Turku, highlighted that elevated MOR levels in anorexia patients result in a significantly different physiological state compared to healthy individuals. This contrasts starkly with findings in obesity cases, where opioidergic activity appears diminished. The intricate balance between hunger, satisfaction, and compulsive eating behavior is influenced by these receptors, providing insight into the possibly maladaptive responses seen in anorexic patients.
Methodology: A Closer Look at the Study
The study’s design involved a comparative analysis of 13 women diagnosed with anorexia nervosa—whose body mass index (BMI) was notably lower than the average—and 13 healthy control subjects matched by age and gender. Utilizing advanced imaging techniques such as positron emission tomography (PET) scans, the researchers meticulously assessed both MOR receptor availability and brain glucose uptake in the participants. Interestingly, despite the undernourished state of the anorexia patients, their brain’s glucose consumption mirrored that of the healthier subjects, suggesting that the brain profoundly prioritizes its energy needs, even at the cost of the body’s overall health.
Professor Lauri Nummenmaa, another key contributor to the study, emphasized that this phenomenon indicates the brain’s remarkable ability to safeguard itself. Even when caloric resourcing is critically low, the brain strives to maintain its functions, thereby raising questions about how compromised bodily states can perpetuate maladaptive patterns of behavior seen in anorexia.
The Role of the Opioid System
Given the observed increase in MOR availability, the study hints that the endogenous opioid system—a network responsible for pain relief, reward, and addiction—could play a crucial role in the etiology of anorexia. This up-regulated opioid response appears to mirror conditions observed in obesity, where MOR functionality is downregulated. The researchers underscore that these findings highlight a dual perspective on appetite regulation, revealing that the nuances of neurobiological responses underpinning disorders like anorexia or obesity are not merely oppositional, but rather indicative of a more complex interplay of hunger and reward pathways.
While the implications of the study are significant, it is paramount to consider its limitations. The female-only cohort necessitates caution in generalizing findings across genders, as anorexia does affect males, albeit less prevalently. Additionally, the sample size raises concerns regarding the robustness of the conclusions, necessitating further research with more diverse and larger participant groups. The absence of detailed questionnaires exploring individual eating behaviors skews the analysis regarding how eating habits relate to changes in MOR availability and metabolic functions.
Furthermore, it remains an open question whether the observed alterations in the opioid system are a primary cause or a secondary effect of anorexia. Future research must address these gaps to enhance our understanding and foster better therapeutic approaches.
The exploration of anorexia nervosa through the lens of neurotransmitter function is a promising step towards demystifying this intricate disorder. As researchers continue to uncover the neural mechanisms at play and the role of neurotransmitters, it is hoped that these insights will pave the way for more effective interventions. The complexity of appetite regulation, reward-driven behaviors, and nutritional needs serves as a clear reminder of the brain’s delicate balance, and enhancing our knowledge is crucial for improving outcomes for those affected by anorexia nervosa. As the investigation into this condition evolves, it is clear that a multifaceted approach encompassing biological, psychological, and social factors will be essential in addressing and treating anorexia effectively.


Leave a Reply