Obesity is a growing global epidemic, with rates nearly tripling in the past five decades. This excessive accumulation of fat in the body not only poses immediate health risks but also increases the chances of developing serious complications such as diabetes, heart disease, and cancer. Scientists have long observed that obesity impairs the function of mitochondria, the “powerhouses of the cell” responsible for generating energy. However, the exact relationship between mitochondrial dysfunction and obesity remains unclear.
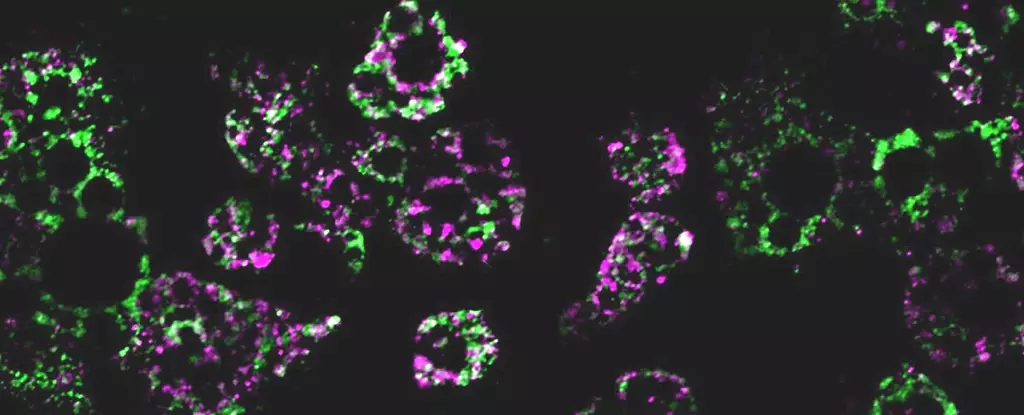
A recent study conducted by an international team of researchers sheds new light on this connection. By investigating the effects of a high-fat diet on mice, the scientists discovered that obesity causes mitochondria within fat cells to fragment into smaller components. These fragmented mitochondria have a reduced capacity for burning fat, contributing to the metabolic imbalances seen in obesity.
The researchers further identified a critical gene involved in this fragmentation process. When they deleted this gene from the test subjects, the mice were able to avoid excess weight gain, even when fed the same high-fat diet. This finding suggests that the gene plays a pivotal role in the transition from a healthy weight to obesity.
The gene in question, known as RalA, controls the breakdown of mitochondria that malfunction. However, when RalA becomes overactive, it interferes with the normal functioning of mitochondria, triggering a metabolic cascade that hampers energy expenditure. By understanding this mechanism, the researchers believe that targeted therapies could be developed to increase fat burning and address weight gain in obese individuals.
While this study provides valuable insights into the role of mitochondria and the RalA gene in obesity, it is important to note that the findings are based on mice models. More research is needed to determine the extent to which these findings apply to humans. Nevertheless, the identification of common proteins influenced by RalA in mice and humans associated with obesity and insulin resistance suggests that the results have relevance in the clinical setting.
These findings have the potential to pave the way for new therapeutic approaches for obesity. By targeting the RalA pathway with novel treatments, it may be possible to address the metabolic dysfunctions and weight gain associated with obesity. However, further studies are warranted to explore the efficacy and safety of such targeted therapies.
The study’s findings underscore the need for a deeper understanding of the complex relationship between obesity, mitochondria, and metabolic disorders. By unraveling the role of mitochondria fragmentation and the involvement of the RalA gene, researchers are a step closer to comprehending the mechanisms underlying obesity and its associated complications.
Obesity is a multifaceted condition influenced by various genetic, environmental, and lifestyle factors. While this study focuses on one specific aspect, it adds to the body of knowledge aimed at devising effective interventions for obesity management and prevention. By exploring the fundamental biology of obesity at the cellular level, scientists can develop targeted therapies that address the root causes of weight gain and metabolic dysfunctions.
The study reveals that obesity induces the fragmentation of mitochondria, impairing their ability to efficiently burn fat. The researchers identify the RalA gene as a critical regulator of this process and suggest that targeting the RalA pathway could be a promising strategy for combating obesity and associated metabolic disorders. While the study’s findings are encouraging, further research is required to fully understand the implications for human health. Nevertheless, this study represents a significant step forward in unveiling the intricate relationship between obesity and cellular physiology. With continued scientific inquiry, future interventions for obesity treatment and prevention may be within reach.

Leave a Reply