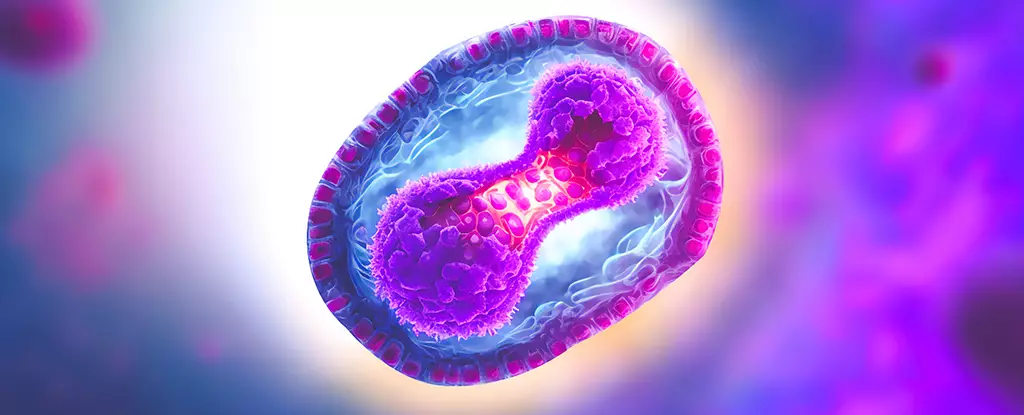
The rise of the new strain of the mpox virus along the eastern border of the Democratic Republic of Congo has sparked concern within the global health community. According to the World Health Organization, this strain is deemed to be the most dangerous variant yet, with evidence suggesting that it can be transmitted not only through sexual contact but also through close skin-to-skin interaction. The demographic being affected by this outbreak has expanded to include schoolchildren, healthcare workers, and entire households. Concurrently, South Africa is also facing an outbreak that has already claimed the lives of three individuals, prompting border authorities to implement rigorous screening measures for travellers entering and leaving the country.
The symptoms of a mpox infection typically begin with nonspecific signs such as fatigue, aches, fever, headache, respiratory symptoms, and a distinct rash. Unlike common viral illnesses, the rash associated with mpox can be itchy, painful, and progresses to fluid-filled blisters that eventually scab over. Transmission of the virus can occur through the sharing of contaminated items like towels or toothbrushes, making it crucial to observe proper hygiene practices. Some infected individuals may present with only a few blisters, which can be challenging to detect depending on their location, while others may remain asymptomatic. Although supportive care forms the basis of treatment for mpox, severe cases may necessitate hospitalization and the use of broad-spectrum antivirals under close monitoring.
Originally identified in laboratory monkeys exported from Africa in the 1950s, mpox, formerly known as monkeypox, transitioned to infecting humans in the 1970s, primarily in the Democratic Republic of Congo. The virus has since evolved and spread across multiple African countries and beyond, garnering global attention in light of rising infection rates. Genetic analysis has revealed that the current outbreak gained momentum in Nigeria around 2016, leading to its eventual declaration as a public health emergency by the WHO in July 2022. Notably, mpox is closely related to other pox viruses like cowpox and the now-eradicated smallpox, the latter of which conferred a degree of cross-protection due to shared genetic similarities.
Despite advancements in understanding mpox, significant challenges persist in combating the virus effectively. The lack of a licensed, mpox-specific vaccine poses a critical obstacle in preventing new infections, particularly among vulnerable populations at higher risk of severe illness and mortality. Efforts are underway to develop tailored vaccines, including an mRNA candidate currently in clinical trials, alongside the exploration of improved treatment strategies. Communication strategies focusing on transmission risks, testing protocols, and destigmatization are vital in promoting public awareness and engagement. Moreover, increased surveillance of animal populations and existing virus variants is essential for early detection and containment of potential outbreaks.
The emergence of the mpox virus presents a multifaceted threat that demands a coordinated and proactive response at the global, regional, and local levels. Through continued research, surveillance, and innovation in vaccine development and treatment options, the healthcare community can mitigate the impact of this evolving pandemic and safeguard public health worldwide.

Leave a Reply