Glioblastoma multiforme (GBM) stands as the most prevalent and lethal form of brain cancer, casting a long shadow over the lives it touches. With an alarming prognosis, patients grappling with this condition often have an average survival time of merely 12 to 15 months post-diagnosis. The statistics are grim, with only 6.9% of patients managing to survive beyond five years, solidifying glioblastoma’s reputation as one of the most inadequately managed cancers in modern medicine. Beyond these dire statistics, the day-to-day experiences of patients can be agonizing; symptoms such as debilitating headaches, seizures, and significant neurological alterations can drastically diminish their quality of life and independence.
Even more sobering is the reality that, despite the urgent need for effective treatments, targeted therapies remain elusive. Historically, standard treatment protocols—surgery, radiation, and chemotherapy—offer only temporary reprieve, often failing to combat the cancer’s formidable resistance mechanisms. Such mechanisms include the tumor’s adept ability to suppress immune responses, compounded by the formidable blood-brain barrier that impedes the efficacy of many therapeutic agents.
The Underlying Biology of Glioblastoma
GBM is classified as a grade 4 tumor by the World Health Organization and is part of a larger group of brain tumors known as gliomas, which originate in the glial cells in the brain and spinal cord. In the UK alone, approximately 3,200 new cases are diagnosed annually, contributing to the larger pool of 12,700 brain and central nervous system tumors reported each year. Globally, the incidence rates hover between 3.2 to 4.2 cases per 100,000 people, summing up to an estimated 150,000 new cases worldwide every year.
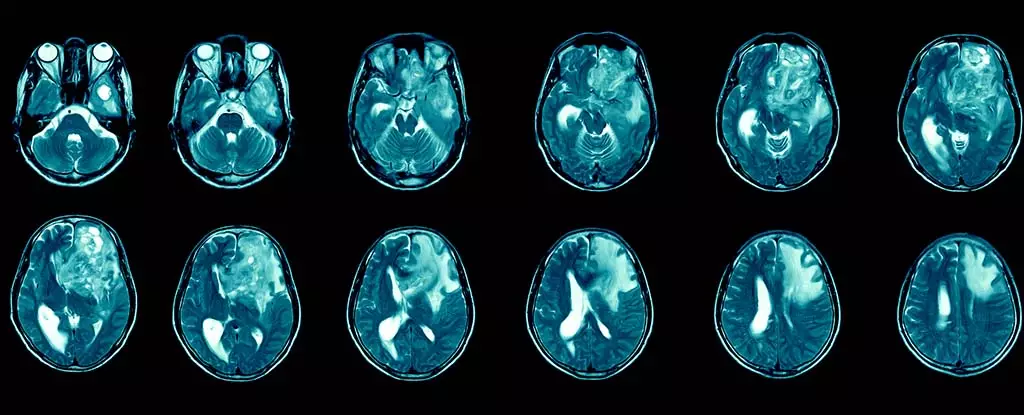
The aggressiveness of glioblastoma is exacerbated by its heterogeneous nature. This complexity manifests in varying genetic mutations across different regions of the tumor, complicating the quest for uniform treatment strategies. As a result, the surgical removal of glioblastomas is often followed by recurrence, posing perpetual challenges not only for patients who must endure this relentless disease but also for oncologists seeking to devise effective interventions.
In light of these challenges, the field of immunotherapy has emerged as a beacon of hope, offering potential new avenues for glioblastoma treatment. This strategy involves harnessing the body’s immune system to identify and target malignant cells, presenting a unique approach to combat what has traditionally been a highly resistant cancer. Despite the complexity of implementing immunotherapeutic modalities, researchers are optimistic about its prospects. Initial clinical trials have indicated that immunotherapy can be effectively administered via injections into the cerebrospinal fluid, heralding a new frontier in treatment delivery.
Yet, developing successful immunotherapy for glioblastoma is not without its obstacles. The adaptive capabilities of the tumor and the varying mutations present create significant challenges in crafting a one-size-fits-all treatment. Nevertheless, researchers are diligently innovating ways to enhance treatment penetration and efficacy, aiming to help patients experience longer, healthier lives.
Despite the exciting advancements, the landscape of brain cancer research has previously suffered from funding shortages, hampering critical innovations. However, a growing wave of initiatives is now recognizing the importance of collaboration across scientific disciplines, encouraging researchers from diverse fields to engage in glioblastoma research. With two decades of experience in understanding immune modulation and its implications in chronic diseases, including a recent focus on Alzheimer’s, important insights are being brought to bear on glioblastoma research.
These multi-disciplinary efforts aim to overcome the current stagnation in treatment development. The collaboration could lead to pioneering discoveries that better navigate the barriers preventing more effective treatments from reaching the tumor sites.
The Path Forward: Challenges and Considerations
While immunotherapy offers tantalizing prospects, it is vital to approach its application in glioblastoma cautiously. Not all cancers demonstrate responsiveness to immunotherapeutic strategies, and patients may experience adverse effects such as organ inflammation. Particularly concerning is the potential for inflammatory responses in the brain; thus, any treatment approaches must carefully consider the risks of exacerbating neurological issues.
Additionally, the method of drug delivery is critical in influencing treatment outcomes. Simpler methods, such as intravenous injections or spinal delivery, pose significantly fewer risks compared to invasive surgical interventions. Researchers are focused on optimizing these delivery methods to minimize patient trauma while maximizing therapeutic benefits.
A Bright Future
Although glioblastoma presents considerable treatment challenges, the expanding interest in immunotherapy spells a hopeful future. As ongoing studies unveil new insights and improved strategies, researchers are eager to unlock more effective treatment pathways for this devastating disease. With increased investment and a collaborative spirit driving innovation, there is renewed optimism that glioblastoma treatments may soon witness a transformative breakthrough, paving the way for a future where quality of life and survival rates could improve for countless patients.


Leave a Reply