Recent advancements in neuroscience have sparked new hope regarding the revival of brain activity following sudden cardiac arrest. A research team in China has achieved a remarkable feat—restoring cerebral function in pigs nearly an hour after circulatory cessation. This finding paves the way for potentially extending the short-lived window for resuscitating patients who experience cardiac arrest. Such breakthroughs necessitate a deeper understanding of the mechanisms involved, and the key appears to involve the liver—a vital organ that plays a crucial role in blood purification.
Sudden cardiac arrest prompts an immediate halt in blood flow, leading to a series of complications commonly referred to as ischemia. Ischemia particularly impacts the brain, where the absence of blood flow can result in irreversible damage in mere minutes. Traditional wisdom dictates that the urgency of resuscitation must occur within a narrow time span, as the multi-organ ischemia complicates the brain’s ability to recover. Previous studies have hinted at the interplay between individual organs during recovery, but research has predominantly focused on the brain itself rather than its relationship with other organs.
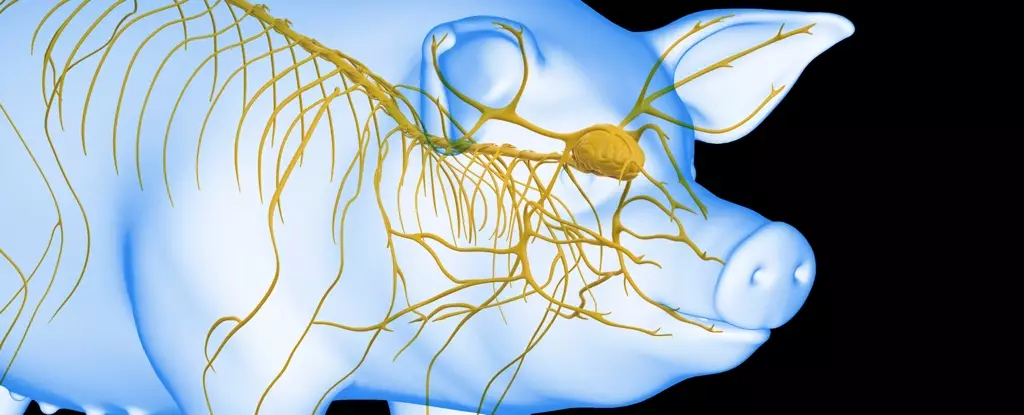
The innovative approach taken by this research highlights the liver’s forgotten role in brain recovery. By employing a well-studied animal model—specifically, Tibetan minipigs—the scientists aimed to elucidate this relationship between organ health and brain functionality following ischemic events.
Led by Xiaoshun He at Sun Yat-Sen University, the team conducted tests with 17 laboratory-raised Tibetan minipigs, systematically examining how the liver’s health affects brain recovery. To dissect this relationship, the researchers subjected two pig groups to brain ischemia for 30 minutes; however, one group simultaneously experienced liver ischemia while the other did not. A control group, which faced no ischemic challenges, served to illustrate the spectrum of brain damage across the different scenarios.
Upon examination of the pigs’ brains after euthanasia, results confirmed a gradation in brain damage aligned with the experimental conditions. Those who had not suffered liver ischemia exhibited notably less brain damage compared to their liver-affected counterparts, prompting further inquiry into the influence of the liver in brain health during ischemic events.
The research progressed into a phase where an undamaged liver was integrated into a life support system designed to revive a brain entirely removed from a euthanized pig. Although this scenario is not indicative of future human treatment, it provided critical data on potential resuscitation timelines. The established life support system involved artificial heart and lung components to sustain blood flow through the brain.
In a fascinating turn of events, the researchers connected brains to this life support system at variable intervals (10, 30, 50, 60, and 240 minutes post-circulation cessation). The addition of a liver into the system revealed promising results: when connected 50 minutes after ischemia, the brain displayed renewed electrical activity that persisted for up to six hours. Conversely, brains deprived of oxygen for 60 minutes showed declining activity, illuminating a pivotal timeframe for effective resuscitation.
The study’s findings underscore the liver’s crucial role in mitigating brain injury following cardiac arrest. As researchers delve deeper into these revelations, they may unlock new pathways that revolutionize emergency medical interventions. The potential to extend the window for successful resuscitation offers newfound hope for patients, potentially improving survival rates and recovery outcomes.
As we look to the future, these groundbreaking insights challenge conventional paradigms regarding organ interaction and recovery. Continued investigation could facilitate the development of advanced life support systems that optimize organ functions post-arrest, further bridging the gap between organ failure and restoration of brain health.
In essence, the Chinese researchers’ discoveries mark a significant leap in our understanding of post-cardiac arrest recovery. By integrating the liver within the resuscitation framework, they have opened the door to innovative strategies that may enhance recovery outcomes not just for animals in research settings but ultimately for human patients at risk of cardiac arrest. The future of cardiac care hangs in the balance, awaiting harnessed breakthroughs that could redefine the extents of medical resuscitation efforts.


Leave a Reply