Cardiac arrest is an urgent medical emergency that can result in death within minutes if not addressed promptly. Cardiopulmonary resuscitation (CPR) is a vital procedure that can significantly increase the victim’s chances of survival by maintaining blood circulation and oxygen delivery to the brain and other essential organs until professional help arrives. Despite its crucial role, emerging research has revealed a concerning trend in the responsiveness of bystanders to perform CPR, particularly towards women. This discrepancy in intervention rates highlights a broader issue of gender bias in emergency healthcare and underscores the need for more inclusive CPR training programs.
The Gender Bias in CPR Intervention
A comprehensive Australian study conducted between 2017 and 2019 revealed alarming differences in how bystanders respond to cardiac arrest based on the victim’s gender. The study analyzed 4,491 incidents and found that a bystander was more likely to administer CPR to men (74%) than to women (65%). This disparity raises critical questions about societal perceptions and training methodologies currently in use. While anatomical differences between male and female bodies do not affect the technique of performing CPR, the hesitation or unwillingness to perform it on women can have life-or-death consequences.
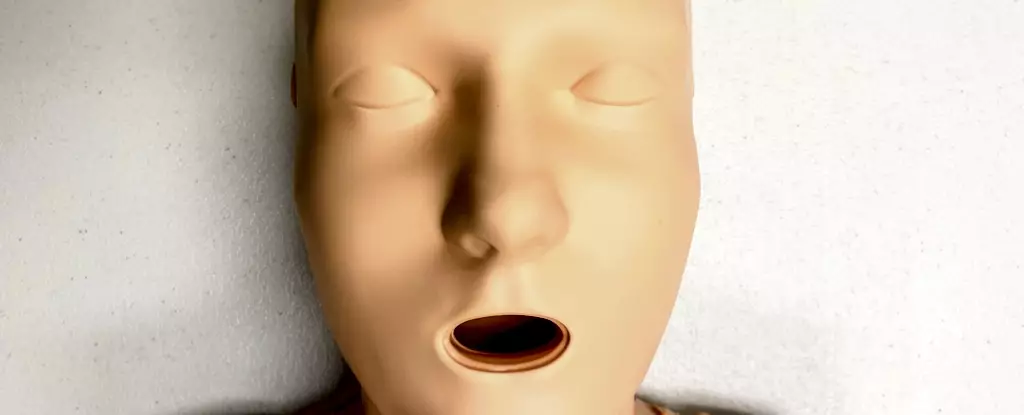
One factor contributing to this hesitation may stem from the design of CPR training manikins, which predominantly feature flat-chested bodies. Research shows that 95% of CPR training manikins lack anatomical features that represent women’s bodies, leading to a “male default” in emergency training. This representation bias could influence bystanders’ confidence and willingness to respond, particularly if they feel uncomfortable or ill-prepared to initiate CPR on someone who looks different from the training manikin.
Statistics corroborate the pressing need for change: women who experience cardiac arrest outside of a hospital setting are 10% less likely to receive CPR compared to their male counterparts. Furthermore, women face higher mortality rates and increased likelihood of severe outcomes such as brain damage following cardiac incidents. This pattern of neglect in recognizing women’s healthcare needs is part of a broader narrative where women’s symptoms are often misdiagnosed or underestimated in medical settings.
The fear surrounding unwanted physical contact further complicates the willingness to perform life-saving measures. Many potential responders may hesitate, fearing accusations of inappropriate behavior or physical discomfort when interacting with someone of the opposite gender. Research indicates that even when trained, individuals in simulated scenarios are less likely to prepare a woman for resuscitation, meaning that the barriers are not solely technical, but deeply rooted in cultural perceptions.
This data strongly suggests that conventional CPR training methods are inadequate in preparing individuals to respond effectively to emergencies involving women. The lack of diverse training resources that reflect the variety of body types—indeed, the sheer absence of breasts on most training manikins—reinforces a societal norm that may cause bystanders to second-guess their instincts in urgent situations. One study noted that out of 20 CPR training manikins available on the market, only five were classified as “female,” and merely one featured visible breasts. This illustrates a glaring oversight in the design of training equipment.
Moving forward, it is imperative for CPR training protocols to incorporate a wider variety of manikins, including those with breasts and diverse body sizes. This adjustment will not only help to prepare individuals more thoroughly for real-life emergencies but can also dismantle the unconscious biases that prevent timely intervention in life-threatening situations.
In addition to revising training resources, greater efforts must be made to educate the public on the signs of cardiac arrest and the critical need for prompt action. The guidelines for performing CPR are straightforward and life-saving; they involve positioning hands correctly on the chest and applying pressure at the appropriate depth and rate. It is essential that bystanders are made aware that the presence of a bra should not delay care, particularly if a defibrillator is necessary.
Ultimately, addressing these disparities in CPR training and emergency response can significantly alter outcomes for women experiencing cardiac arrests. Progress in this field requires collective efforts towards inclusivity in training materials and a commitment to public education that acknowledges women’s unique health risks. To equip bystanders with the confidence to act, we must challenge and change the norms that marginalize women’s health in emergencies. In doing so, we can ensure that life-saving measures are not hindered by gender biases, ultimately fostering a society where every life is valued equally.
Leave a Reply