Cancer remains a formidable adversary in the modern medical landscape, prompting researchers to explore every avenue that might enhance treatment efficacy. Recent efforts have illuminated an unexpected aspect of immune response in patients undergoing immunotherapy, revealing a complex interplay that may dramatically improve survival rates. The findings from two significant studies suggest that tapping into a duality in immune responses—termed “yin and yang”—might unlock the potential for more effective cancer treatments.
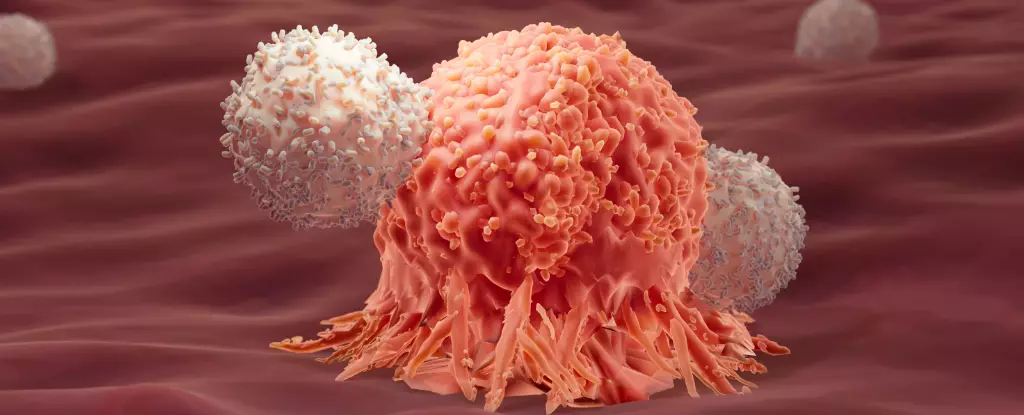
Immunotherapy has emerged as a groundbreaking approach to treating various cancers by leveraging the body’s natural defenses. This innovative method often utilizes techniques like CAR-T cell therapy, where T cells are extracted from a patient, genetically modified to target cancer cells, and then reintroduced into the bloodstream to mount an attack against malignant growths. While immunotherapy has shown great promise, particularly in treating certain types of blood cancers such as acute lymphocytic leukemia (ALL), it is not without its limitations. A staggering proportion of patients experience relapse within a year of treatment, highlighting the need for deeper investigation into why some patients achieve long-term remission while others do not.
The research led by experts at the École Polytechnique Fédérale de Lausanne (EPFL) targeted this very issue, aiming to uncover unique characteristics of immune cells in patients who enjoyed prolonged remission. By meticulously analyzing data from initial clinical trials involving CAR-T therapy, researchers constructed a genetic map of nearly 700,000 CAR-T cells, identifying patterns that suggested an unconventional immune response profile linked to sustained success.
Traditionally, the immune system’s type 1 response has been considered crucial in identifying and combating intracellular threats, including cancer. This perspective has dominated the narrative around immunotherapy, which primarily focuses on enhancing type 1 responses. However, the remarkable findings from recent studies point to the potential significance of type 2 immune responses, generally associated with combating larger threats, such as parasitic infections. The key revelation is that these so-called type 2 markers were prominently featured in patients who remained cancer-free for years following treatment.
This portrayal stands in stark contrast to established beliefs about type 2 responses as merely ancillary or even detrimental in the context of cancer. By revealing a correlation rather than direct causation, the studies pave the way for an intriguing hypothesis: there exists a synergistic relationship between type 1 and type 2 immune responses that can be harnessed to optimize therapeutic outcomes.
The second study further delved into these findings by experimenting with mouse models of colon adenocarcinoma—solid tumors notoriously resistant to standard immunotherapy. The researchers employed a dual-approach strategy, administering both type 1 and a modified type 2 immune response. The results were striking: an astounding 86% of the mice receiving the synergistic treatment were eradicated of their tumors, compared to a dismal outcome for the group receiving type 1 therapy alone, which faced complete failure within weeks.
What made the difference? The modified type 2 immune proteins appeared to enhance the cells’ metabolic capacity, particularly through a process known as glycolysis, thus providing T cells with the necessary energy to persist in their fight against cancer. This metabolic boosting is crucial, as immune cell exhaustion is a significant obstacle in cancer treatment.
These groundbreaking studies invite a reevaluation of how we approach cancer immunotherapy. By recognizing the complementary dynamics of different immune responses, researchers can design more robust treatment regimens that exploit this duality. This approach could extend beyond just enhancing existing therapies; it might redefine our understanding of what constitutes an effective immune response against cancer.
The potential translation of these findings from animal models to human cases presents additional layers of complexity. While the results are promising, researchers emphasize that the correlation found in the studies necessitates further exploration. Future clinical trials will be critical in determining the viability of integrating type 2 immune responses into conventional immunotherapeutic strategies for cancer treatment.
As cancer research continues to unfold, the integration of novel insights, such as the interplay between distinct immune responses, represents a significant leap forward in therapeutic potential. By harnessing the synergy of immune responses described as “yin and yang,” the medical community stands on the cusp of possibly revolutionary advancements in cancer care. The journey from hypothesis to clinical application may take time, but the determination to expand our understanding of immunology could ultimately reshape the landscape of cancer treatment, transforming once daunting prospects into beacons of hope for patients around the globe.

Leave a Reply