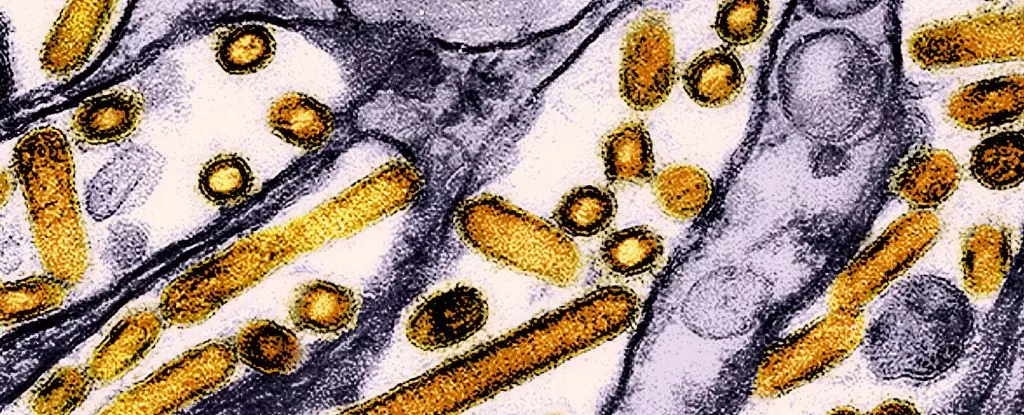
The recent findings concerning the transmission of highly pathogenic avian influenza (HPAI) among dairy workers present a troubling expansion of our understanding of zoonotic diseases. A study conducted by the Centers for Disease Control and Prevention (CDC) sheds light on the presence of antibodies related to the virulent H5N1 strain in individuals who had direct contact with infected cattle. The findings, which indicate an alarming yet largely asymptomatic spread among a sample group of 115 dairy farmers in Michigan and Colorado, signal a pressing need for rigorous monitoring and strategic health interventions.
Unrecognized Infection and Its Implications
Between June and August 2024, the CDC discovered that approximately 7% of the tested dairy workers exhibited antibodies associated with HPAI H5N1. This suggests that while the majority of infections observed in this demographic were mild or asymptomatic, the lack of detectable illness is misleading; it thinly veils the potential threat such infections represent. The essential takeaway here is that while individuals may not exhibit severe symptoms, the virus’s capacity for mutations poses unique public health challenges. In particular, the current situation underscores an important paradox: fewer symptoms can lead to a greater risk of transmission, as individuals may unknowingly facilitate the spread of the virus without employing necessary precautions.
One particularly concerning aspect of this situation is the divergence of avian influenza strains. Reports from Cambodia highlight a lethal outbreak involving a hybrid strain of H5N1 that has exhibited mutations promoting both aerial transmission and mammalian infection. How easily a virus like H5N1 can mutate in response to selective pressures like environmental changes or human intervention cannot be overstated. The emergence of this novel strain, which resulted in the deaths of three individuals, draws attention to the critical importance of a proactive approach in monitoring the virus, especially amidst rising concerns about virulent mutations.
The relationship between human and animal health is made all the more apparent by the recent data that emphasizes the presence of H5N1 antibodies in dairy workers, who often handle infected cattle without appropriate personal protective equipment (PPE). As reported, none of the workers with detectable antibodies adhered to recommended PPE guidelines, highlighting significant lapses in safety protocols that could place them—and, consequently, the general public—at grave risk. Enhanced education initiatives emphasizing the importance of protective measures are needed, particularly considering the linguistic diversity among the worker population.
The CDC’s findings reveal a troubling reality: without stringent health measures, the bird flu is increasingly likely to breach species barriers. The case of a critically ill teenager in Canada serves as a critical example of how rapidly the strain can adapt, as initial genetic sequencing indicates a modification enhancing its ability to infect humans. Such developments amplify the urgency surrounding public health protocols and proactive monitoring. The spatial and temporal dynamics of the outbreaks necessitate a unified response from health organizations worldwide.
As outbreaks spread across the United States—impacting over 400 dairy herds across 48 states—authorities are reminded of the gravity of surveillance in managing zoonotic diseases. More than 90 million domestic birds have already been culled due to this silent encroachment of HPAI. The strategy to control this disease must include heightened public awareness and prompt reporting of sick or deceased birds, thereby facilitating rapid response and containment measures.
Given that HPAI presents distinct symptoms in animals—drowsiness, coordination issues, and unusual behavior—educating the public on recognizing these signs can prove invaluable. The integration of such information into community outreach programs, specifically tailored for vulnerable populations, can help mitigate the risks associated with both animal and human health.
Furthermore, the need for advancing research into vaccines for both humans and wildlife has never been more urgent. The preliminary efforts to vaccinate California condors signify a proactive approach to protect endangered species, which may hold critical ecological roles. Continual investment in research, education, and policy reform will be crucial to address the dual challenges posed by avian influenza in both agricultural settings and natural ecosystems.
As the world grapples with emerging infectious diseases, the case of HPAI H5N1 among dairy workers illustrates the complex interplay of zoonotic transmission and public health. Vigilance is critical as we move forward; the continued spread of H5N1 serves as a harbinger, alerting us to the potential human health crises that may lie ahead if proactive measures are not implemented urgently and effectively.

Leave a Reply