Alzheimer’s disease is a devastating neurodegenerative disorder that primarily affects brain tissue, particularly areas crucial to memory. It remains a significant challenge for researchers to identify the exact triggers and cascade of effects responsible for the damage caused by Alzheimer’s. While previous studies have focused on the immune system’s role within or near the brain, little attention has been devoted to exploring potential differences in white blood cells throughout the rest of the body. However, a recent study conducted by researchers from Northwestern University in the US sheds light on an intriguing aspect of immune cell behavior in Alzheimer’s patients.
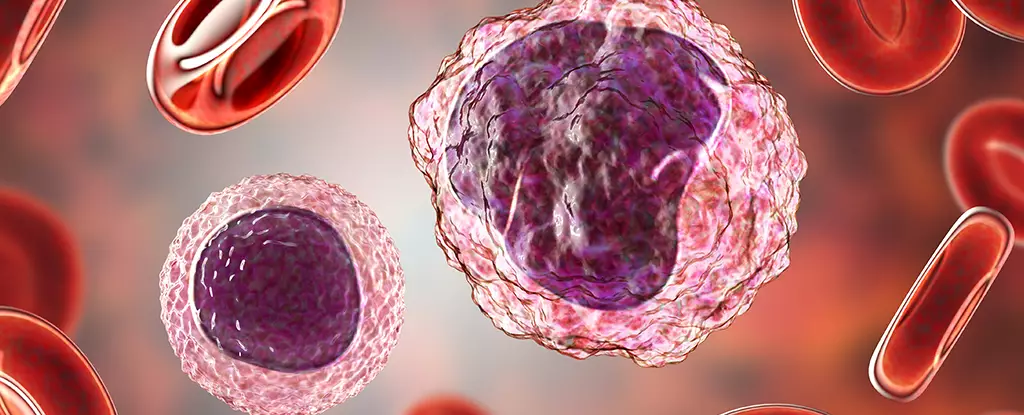
To investigate the potential involvement of peripheral immune cells in Alzheimer’s disease, neurologist David Gate and his team employed single-cell gene translation technology. They analyzed individual white cells taken from both healthy participants and individuals diagnosed with Alzheimer’s disease. The study revealed that every type of white cell in Alzheimer’s patients harbored epigenetic changes—alterations in DNA chemistry that can affect gene expression.
Researchers discovered that sections of DNA in peripheral immune cells from Alzheimer’s patients unwind in a specific manner, exposing genes with the potential to trigger a response within the brain. These changes in the DNA sequences allowed genes to be read more easily, potentially influencing the progression of Alzheimer’s disease. The study’s findings suggest that the peripheral immune response may have implications for Alzheimer’s disease risk.
In the study, researchers noticed distinct changes in various types of white blood cells in individuals with Alzheimer’s disease. Monocytes, which are large white cells, exhibited epigenetic changes that depended on their apolipoprotein E genotype—a combination of genes that affects an individual’s risk of developing Alzheimer’s. Another type of white blood cell, the CD8 T cell, also showed differences in individuals with Alzheimer’s. These T cells displayed key epigenetic changes that caused a membrane protein called CXC motif chemokine receptor 3 (CXCR3) to stand out more prominently. This protein plays a role in guiding the T cells to the brain.
The reason behind the specific functioning of T cells, particularly their attraction to the brain, remains unclear. However, researchers speculate that damaged brain tissue emits a signal that attracts T cells through the CXCR3 antenna. While T cells can be toxic to the brain, it is unclear whether they are attempting to repair the damage or contribute to further complications in Alzheimer’s disease.
Understanding the emergence and implications of these epigenetic changes is a topic for future research. However, the knowledge that such changes exist opens up new possibilities for deeper insights into the progression of Alzheimer’s disease. Additionally, this research could potentially identify new therapeutic targets for the development of treatments.
The study conducted by researchers from Northwestern University sheds light on the role of immune cells in Alzheimer’s disease. The findings indicate that peripheral immune cells in Alzheimer’s patients exhibit subtle changes to how their genes are read, suggesting a potential connection between the immune response and disease development. The different types of white blood cells found in Alzheimer’s patients show epigenetic changes that could influence the disease’s progression. Further research is necessary to fully understand the underlying mechanisms and therapeutic possibilities. However, these findings have promising implications for future advancements in the field of Alzheimer’s disease research.

Leave a Reply