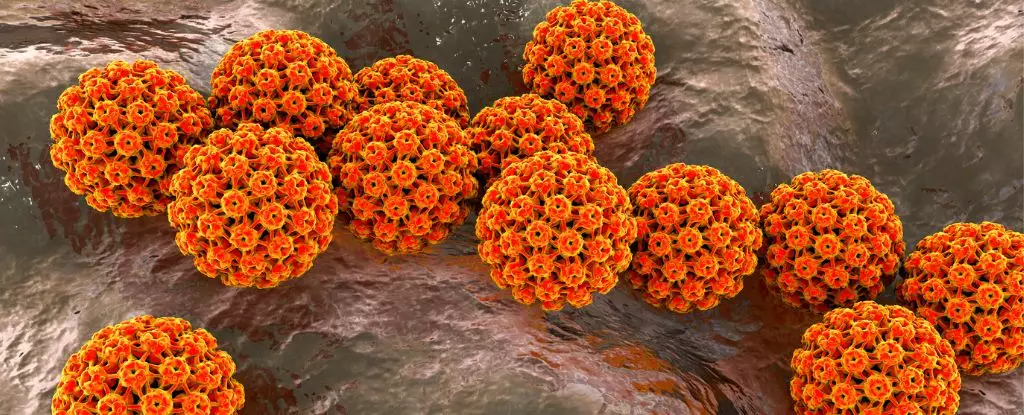
Recent research has highlighted a pressing public health concern: men are vulnerable to dangerous forms of oral human papillomavirus (HPV) throughout their lives. This threat is not just confined to younger populations but extends to middle-aged men who may have missed earlier vaccination opportunities. The implications of these findings are profound, particularly in light of the rising incidence of oropharyngeal cancers across regions like the United States and Europe. These cancers, originating in the throat and mouth, present a significant risk to men, who are diagnosed with them at a much higher rate than women, even in the absence of conventional risk factors such as smoking or heavy drinking.
Determining the Risk Factors
A pivotal study involving over 3,000 healthy men aged between 18 and 70 has illuminated the continuous nature of HPV risk across the lifespan. Researchers discovered that age does not significantly influence the likelihood of acquiring new, cancer-causing strains of HPV; men remain susceptible throughout their lives. This continuous vulnerability raises critical questions about current HPV vaccination policies, which predominantly target younger demographics. Strains such as HPV-16 and HPV-18 are notorious for their association with nearly 90 percent of oral cancer cases. Yet, vaccination rates among young males are alarmingly low compared to their female counterparts, which could elucidate the ongoing rise in oropharyngeal cancers.
Vaccination Policies and Challenges
The recommendations from the U.S. Centers for Disease Control and Prevention (CDC) advocate for the vaccination of all individuals up to the age of 26. However, for men over this age, vaccination is only advised for those who are immunocompromised or possess other risk factors. The prevailing rationale suggests diminished efficacy in this older cohort due to a higher likelihood of prior HPV exposure. Yet, emerging evidence challenges this assumption. Previous studies have primarily focused on men with male sexual partners, neglecting the full spectrum of HPV transmission routes—oral sex isn’t the sole means of infection; contact via fingers and skin can also facilitate transmission.
Led by experts at the Moffitt Cancer Center in Florida, the recent study collected oral gargle samples from participants over several years. Remarkably, nearly 20 percent of the participants had an existing oral HPV infection at the beginning of the study period, with 6 percent of them carrying strains known to cause cancer. This data underscores the pervasive nature of HPV and highlights the necessity for ongoing public health initiatives aimed at raising awareness about the risks associated with HPV, particularly within male populations.
The findings emphasize the need for tailored vaccination strategies that consider regional variations in HPV prevalence and the transmission mechanisms that contribute to its spread. According to epidemiologist Anna Giuliano, it is crucial to maintain awareness and vigilance against oral HPV infections, particularly as the risk factors for strains like HPV-16 appear to compound with age. Factors such as alcohol consumption and sexual behavior—including the number of male and female partners—are intricately linked to the increased risk of contracting oral HPV.
As we grapple with the implications of this research, it is clear that public health initiatives must evolve. There is an urgent need to disseminate crucial information about HPV vaccination beyond the confines of youth and to engage middle-aged men in health dialogues. As the landscape of HPV-related risks grows increasingly complex, so too must our strategies in vaccination and education. Addressing this silent threat with robust awareness and proactive measures could significantly curb the rising tide of HPV-associated cancers and save countless lives in the process. The battle against HPV is not just a women’s issue; it’s a shared responsibility that demands a collective response.

Leave a Reply