The intricate relationship between hormonal fluctuations and their effects on the human body is a phenomenon that has long piqued the interest of scientists. Recent research has further illuminated this relationship, specifically examining how the hormonal changes involved in the menstrual cycle influence brain structure and functionality. A profound study undertaken by neuroscientists at the University of California, Santa Barbara, led by Elizabeth Rizor and Viktoriya Babenko, aims to bridge the gap in our understanding of these physiological changes—not only within reproductive systems but throughout broader neurological contexts.
The menstrual cycle, an experience that forms a significant aspect of life for individuals who menstruate, unfolds over approximately 28 days and is characterized by a series of hormonal fluctuations. These variations have historically been linked more frequently to reproductive health than to cognitive or neurological changes. However, the groundbreaking study referenced here shifts focus, offering insights into how these hormonal oscillations might reshape the brain, suggesting a far-reaching interconnection between the endocrine and central nervous systems.
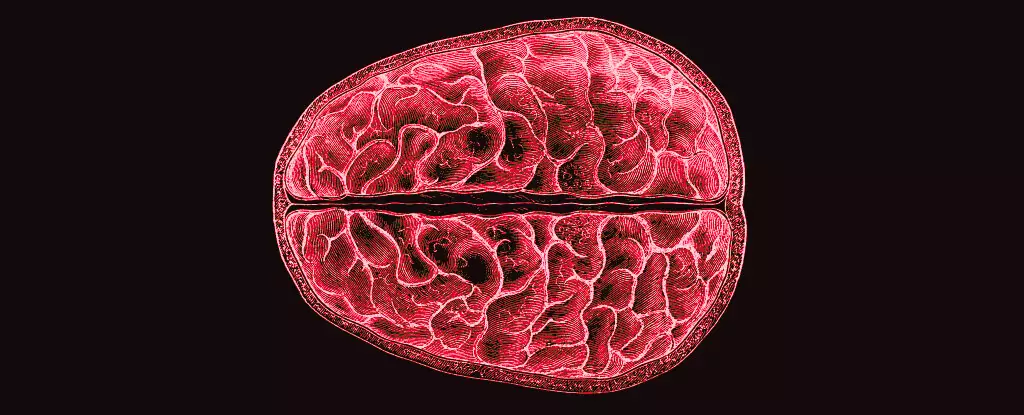
To investigate the potential impact of menstrual cycles on brain structure, the research team employed magnetic resonance imaging (MRI) technology to capture detailed brain scans of 30 female participants at different phases of their cycles—specifically during menstruation, ovulation, and the mid-luteal phase. Simultaneously, the team measured the participants’ hormone levels, seeking to draw correlations between hormonal changes and observable structural brain changes.
Previous studies have primarily focused on how hormones influence cognitive processes, often neglecting the more subtle yet crucial structural changes occurring in the brain. This research, therefore, represents a significant advance toward understanding the vast implications of hormonal shifts. As the researchers aptly noted, the hormonal rhythms inherent in the menstrual cycle have profound effects on behavior and brain structure, yet much remains unexplored concerning the microstructural changes that accompany these hormonal transitions.
The results of this research illuminated a fascinating dynamic: fluctuations in hormones like estradiol, luteinizing hormone, and progesterone correlated with shifts in both gray and white matter volumes within the brain. Notably, white matter experienced changes that suggested enhanced information transfer just prior to ovulation, a critical period when specific hormones surge. Meanwhile, progesterone, which rises in the latter half of the menstrual cycle, was associated with increased tissue volume and a reduction in cerebrospinal fluid.
Such findings are vital as they lay foundational groundwork for further inquiry into how menstrual cycles could influence mental health. While this study did not provide direct answers to the effects these changes have on cognition or emotional well-being, it raises pressing questions about why individuals who menstruate often encounter psychological distress linked to their cycles. The knowledge that structural brain changes coincide with fluctuating hormone levels could be instrumental in addressing menstrual-related mental health disorders, thus opening avenues for future research and potential clinical interventions.
Despite the importance of this subject matter—impacting roughly half of the global population for a significant portion of their lives—research on menstruation has historically lagged. Often relegated to anecdotal evidence and minimal scientific scrutiny, understanding the full scope of menstrual health, including psychological and neurological dimensions, remains an unfinished chapter in medical literature.
Therefore, initiatives such as the one led by Rizor and Babenko are essential in driving forward our comprehension of how hormonal shifts uniquely shape not just reproductive health but overall psychological well-being. As our understanding of these mechanisms deepens, it may foster a healthier and more informed discourse on menstrual health, ultimately leading to improved strategies for managing associated mental health challenges.
In essence, this research represents a critical leap in recognizing the interdependent relationship between hormonal cycles and cognitive functions, urging both scientists and clinicians to explore these connections further. As our understanding of these dynamics grows, it is imperative that we advocate for expanded research efforts aimed at unveiling the complexities of how our biology shapes our experiences and responses. The journey toward comprehensive menstrual health awareness is far from over, yet studies like this pave the way for informed dialogue and enhanced health strategies for individuals throughout their reproductive years.


Leave a Reply