The ongoing debate surrounding the use of selective serotonin reuptake inhibitors (SSRIs) in treating mood disorders is marked by contrasting opinions and a lack of comprehensive understanding about their efficacy and mechanisms. Recent research led by Vibeke Dam and her colleagues at Copenhagen University sheds new light on how SSRIs like escitalopram affect cognitive abilities, particularly in individuals suffering from moderate to severe depression. This article explores the findings from the study, the implications for treatment, and the broader context of SSRI use in mental health care.
In an effort to evaluate the cognitive effects of SSRIs, the researchers meticulously designed a study involving 90 participants diagnosed with significant depressive symptoms. By conducting brain scans and cognitive assessments before starting treatment and after an eight-week period on escitalopram, the team aimed to understand the drug’s potential changes on brain function and mood. The decision to focus on a medication with a long-standing history of clinical use provided a pragmatic backdrop for assessing the nuanced relationship between receptor activity and cognitive enhancement.
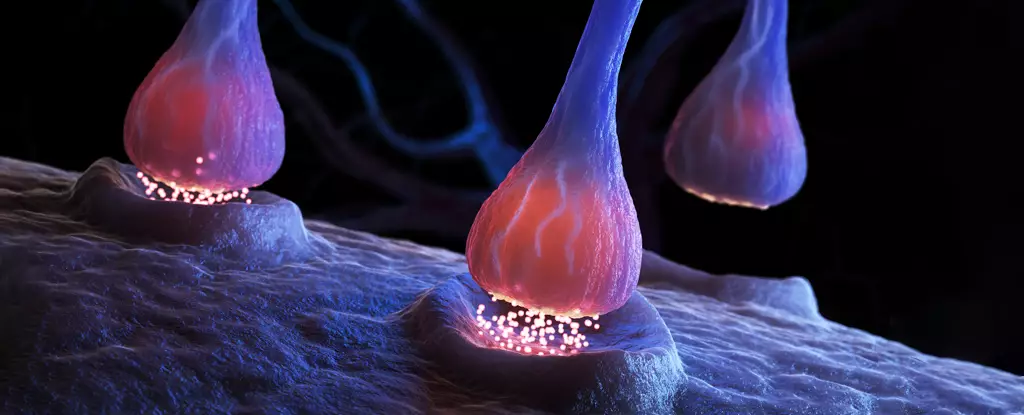
Once participants began the daily regimen of the SSRI, they underwent another set of evaluations after the treatment phase. Interestingly, significant reductions were observed in the serotonin receptor binding, specifically a 10 percent decrease in available receptors. This drop indicates a possible adjustment in the brain’s chemistry and raises questions about how such a shift could offer improvements in cognitive abilities, particularly verbal memory.
The study findings revealed that participants exhibited notable improvements in memory assessments, especially concerning their ability to recall specific words. Notably, those displaying minimal change in the 5-HT4 serotonin receptor, a target of the SSRIs, demonstrated the most pronounced enhancements in verbal memory. This observation suggests a potential link between receptor stability and cognitive function, indicating that the remaining receptor activity may become more efficient in the presence of elevated serotonin levels in the brain’s synapses.
Vibeke Dam points to this dynamic interaction by stating, “Our work ties the improvement in cognitive function to the specific 5-HT4 receptor,” highlighting how optimizing antidepressant treatment could potentially pivot towards direct stimulation of this receptor. This insight opens new avenues for research focused on cognitive outcomes for individuals suffering from depression.
Despite the observable cognitive enhancements, a paradox emerges: the improvements in mood did not correlate with changes in the 5-HT4 receptors. This discrepancy raises critical questions regarding the actual therapeutic value of SSRIs in alleviating depressive symptoms. The skepticism surrounding SSRIs is underscored by findings from various studies that challenge the notion of serotonin’s primary role in the pathology of depression. As the evidence mounts, researchers and clinicians are left to grapple with the ramifications of these contradictions and what they mean for future treatment paradigms.
Vibe Froekjaer, a neurobiologist involved in the study, cautions that while advancements in cognitive function provide a promising direction, the ethical constraints of the study—most notably the absence of a placebo group—complicate the interpretations of results. The concern remains that improvements may be attributed to factors outside the SSRI’s influence, necessitating further investigation.
As antidepressants continue to play a pivotal role in mental health treatment, it’s crucial to assess their validity comprehensively. The increasing scrutiny on SSRIs, coupled with emerging skepticism about their effectiveness compared to placebos, necessitates a reevaluation of treatment strategies for mood disorders. Importantly, patients are advised against abruptly discontinuing SSRIs without medical supervision, given the possible adverse effects and withdrawal symptoms.
The synthesis of cognitive and mood findings underscores the importance of ongoing research into the mechanisms of SSRIs and other antidepressants. Understanding how different receptors influence cognitive functions independent of mood could reshape the therapeutic landscape for individuals grappling with depression.
Research in this area is still in its infancy, and as highlighted by the Copenhagen team, future studies are essential to unravel the complexities of antidepressant action. As we strive for advancements in precision psychiatry tailored to individuals with mood disorders, increased knowledge about the biochemical pathways and cognitive implications of treatments will be fundamental. Given the substantial reliance on SSRIs, the quest for clarity in how these medications operate remains critical for informed clinical practice and enhanced patient outcomes.
While SSRIs have been mainstays in treating depression, the nuanced relationship between receptor dynamics and cognitive improvement demands further exploration. The field of psychiatry stands at a crossroads where more refined approaches could potentially elevate the standards of care for those in need.
Natural gas leaks are a growing concern in both urban and rural settings, with potential…
Recent groundbreaking research at the University of Vienna has unveiled a novel interplay of forces…
In recent years, perovskites have garnered significant attention in the fields of materials science and…
For decades, astronomers have probed the depths of the Milky Way, grappling with two perplexing…
Foreign direct investment (FDI) in developing nations has long been heralded as a path to…
As spring beckons in April and May, stargazers have the unique opportunity to witness nature's…
This website uses cookies.