Recent advancements in pharmaceutical treatment have brought hope to Alzheimer’s disease patients, offering the potential for extended independence. Yet, as promising as these innovations appear, the reality is layered with complexity, particularly regarding gender differences in drug efficacy. New studies have emerged highlighting critical discrepancies in how male and female brains respond to novel Alzheimer’s treatments, raising urgent questions about inclusivity in clinical research.
Lecanemab, an intravenous therapy that recently gained FDA approval, showcases remarkable potential. A phase 3 clinical trial known as CLARITY AD reported a 27 percent reduction in cognitive decline among those treated with the drug compared to a placebo. This finding, along with the political weight of the FDA’s backing, lends credibility to the drug as a viable treatment option. However, emerging analyses remind us to dissect these results further, as they reveal a significant disparity in effectiveness based on sex. Males exhibited a striking 43 percent decline in cognitive deterioration, while females experienced only a 12 percent slowdown, a statistic that, while not statistically significant, highlights potential inequities in treatment outcomes.
Despite the excitement surrounding Lecanemab, it is crucial to recognize the cautionary interpretations emerging from recent studies. Notably, researchers have found that the initial findings may indicate either limited effectiveness or negligible benefits for women. A closer examination of the trial data reveals an alarming 31 percent gap in therapeutic response. Although this difference did not emerge as statistically significant across various simulations, it evokes genuine concern among scientists exploring gender factors in drug effectiveness. The exploration of sex-related outcomes in clinical trials has historically lagged, contributing to significant blind spots in understanding how unique biological factors influence treatment responses.
Marina Lynch, a neuroscientist from Trinity College in Ireland, urges that the time has come to prioritize gender in clinical studies. Only 5 percent of published neuroscience research as of 2019 examined sex differences, revealing a serious oversight that may have far-reaching consequences. Ignoring these disparities not only endangers female health but also hampers the progress of overall medical knowledge. The necessity for trials to adequately recruit and evaluate both male and female participants cannot be overstated; integrating this rigor into research design is crucial for uncovering how treatments operate across diverse patient populations.
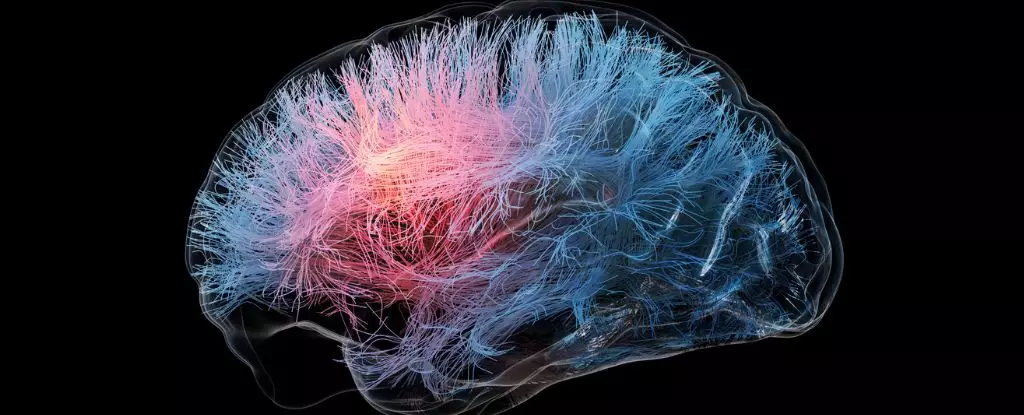
The interaction of sex hormones and chromosomes with brain health and Alzheimer’s pathology cannot be ignored. Findings suggest that women’s unique biological makeup may influence how effective amyloid-targeting drugs like Lecanemab are, driving the need for comprehensive analyses that delve deeper into these mechanisms. If the heterogeneous nature of Alzheimer’s is to be adequately addressed, broader research agendas must be enacted that consider how factors such as sex can modulate the effectiveness of treatment strategies.
Despite years of emphasis on amyloid plaques as a primary cause of dementia, recent research questions the reliability of these markers as predictors of cognitive decline. Studies reveal that a substantial subset of patients previously diagnosed with Alzheimer’s may lack amyloid plaques entirely. This inconsistency, paired with concerns over how amyloid-targeting therapies function differently in males and females, indicates the need for a paradigm shift in Alzheimer’s research. Acknowledging that treatment efficacy may not rely solely on amyloid presence but also on biological and gender-based variations can lead to more personalized, effective therapies.
The path forward should be paved with collaboration among scientists, clinicians, and pharmaceutical developers to share data and insights gleaned from recent trials. By pooling resources and knowledge, researchers can explore gender differences more comprehensively, fostering innovative approaches that prioritize the unique needs of both men and women. The urgency of addressing these disparities in Alzheimer’s treatment cannot be overstated; tailored strategies may be the key to unlocking improved health outcomes for millions battling this devastating condition.
In the race against Alzheimer’s disease, acknowledging and addressing gender disparities holds promise for not only enhancing treatment efficacy but also transforming the lives of countless individuals affected by this condition. The scientific community stands at a pivotal juncture where a concerted effort can deliver profound change—one that brazenly champions the importance of diversity in research and treatment protocols for the future.
In an era where environmental degradation and climate change are pressing concerns, the quest for…
In a stunning revision of astronomical history, recent research has unearthed compelling evidence suggesting that…
Recent research spearheaded by scholars from MIT highlights a critical yet often overlooked facet of…
In our society, the pursuit of thinness has often overshadowed the importance of overall health…
Aging is an inevitable aspect of life, and while it brings a wealth of experience,…
In the rapidly advancing field of photonic computing, a group of researchers from the University…
This website uses cookies.